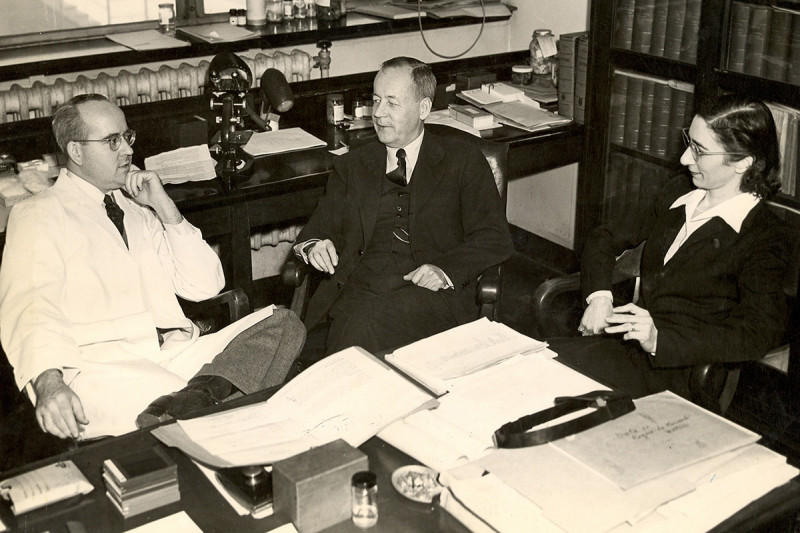
From left: Then Chair of the Department of Pathology Frank Foote, Jr.; Fred W. Stewart; and Sophie Spitz. Dr. Spitz was most famous for her discovery of juvenile melanoma, which is now known as Spitz nevi.
The Fred W. Stewart Award of Memorial Sloan Kettering Cancer Center honors a pathologist each year who has made outstanding contributions in advancing our knowledge of human cancer.
The Award emphasizes the clinical significance of those contributions, particularly in diagnosis and patient care. It reflects the traditions and values brought to the Department of Pathology by Dr. Stewart, first as an Associate of Dr. James Ewing, and then as Chairman of the Department, for a period extending more than 30 years.
2019 Recipient
Linda Ferrell, MD
Linda Ferrell is the 2019 recipient of the Fred W. Stewart Award, given annually by Memorial Sloan Kettering’s Department of Pathology to an individual who has made outstanding contributions to the understanding of human neoplastic disease.
Dr. Ferrell is a world-renowned liver pathologist. Her stellar career achievements exemplify how dedicated surgical pathologists can have a momentous impact on the field of medicine.
Dr. Ferrell obtained an MD degree from the University of Kansas, where she also completed pathology residency training. She did fellowship training at the University of California, San Francisco (UCSF), then joined the faculty there, remaining at the university until 2015, when she retired to emeritus status. Over the years, Dr. Ferrell has served in multiple important roles at UCSF, including as the distinguished professor in anatomic pathology (endowed chair), vice chair of clinical affairs in the department of anatomic pathology, director of surgical pathology (2000 to 2015), director of the surgical pathology fellowship (2000 to 2014), and director of the liver and gastrointestinal pathology fellowship (2005 to 2014). At the national and international level, Dr. Ferrell has also played important roles: She is a past president of the Hans Popper Hepatopathology Society (2008 to 2009) and the United States and Canadian Academy of Pathology (USCAP) (2012 to 2013).
Dr. Ferrell has devoted her academic career to the study of liver pathology. As evidenced by her numerous publications (more than 200 original articles), she has made great contributions to the understanding of the pathology of liver tumors, particularly of well-differentiated liver tumors, including hepatocellular adenoma variants, focal nodular hyperplasia-like lesions, vascular lesions, and malformations in the liver. Through participation in major organizations, such as the Clinical Research Network in Nonalcoholic Steatohepatitis (a National Cancer Institute–sponsored consortium) and the International Liver Pathology Study Group (of which she was a founding member), Dr. Ferrell worked relentlessly to ensure the most effective integration of pathology into the various studies of liver diseases. Her seminal works on liver pathology in recurrent hepatitis C after transplantation and on the diagnosis of dysplastic nodules have gained worldwide attention, and a number of these studies have been recognized internationally as leading papers in the field.
Dr. Ferrell is also an ardent educator. She has nurtured generations of pathology residents and fellows. She chaired two major annual courses for pathologists for multiple years: at UCSF for 33 years and for the California Society of Pathologists for eight years. Through the years, she has served a wide variety of teaching roles via USCAP. Her numerous book chapters and major liver pathology textbooks (including the premier text, MacSween’s Pathology of the Liver, fifth, sixth, and seventh editions) have benefitted liver pathologists everywhere. Her contribution as the lead editor of Liver Pathology (part of the consultant pathology series from Demos Publishers), which emphasizes difficult diagnostic problems in liver pathology, has similarly offered invaluable guidance. Dr. Ferrell has lectured extensively both nationally and internationally. Her lectures are always very well received.
It is no surprise that numerous awards have been bestowed on Dr. Ferrell in recognition of her achievements. These include the 2008 Gold Headed Cane Award, the 2015 F. K. Mostofi Distinguished Service Award from USCAP, the 2016 Harvey Goldman Master Teacher Award from USCAP, the 2017 President’s Award from the Arthur Purdy Stout Society of Surgical Pathologists, and numerous UCSF teaching awards for resident and medical student teaching.
Today, as we celebrate the memory of Dr. Stewart, a man who early on brought surgical pathology to the front lines of oncology, it is most fitting that the medal in his name be given to an individual who has dedicated her career to the practice of surgical pathology and contributed monumentally to the continued advancement of this discipline in modern times. We congratulate Dr. Ferrell on this well-deserved award.
2018 Recipient
Jonathan I. Epstein, MD
Dr. Jonathan I. Epstein is the recipient of the 2018 Fred Waldorf Stewart Award, bestowed annually by the Department of Pathology at Memorial Sloan Kettering Cancer Center on an individual who has made outstanding contributions to our understanding of human neoplastic disease. Dr. Epstein is a world-renowned pathologist who has devoted his academic career to the study of urologic pathology and its clinical correlates. While his name is synonymous with every major academic effort in the GU Pathology community over the past three decades, including editorship of and significant contributions to the 2004 and 2016 World Health Organization GU tumor classification, he is best known for his work in prostate pathology spanning all major aspects of the disease. As the convener and major force behind the 2005 and 2014 conferences on prostate cancer grading, Dr. Epstein is considered the international authority on the subject. Importantly, his recent efforts to gather and publish large multi-center, international data sets supporting the concept of Prognostic Grade Grouping for prostate cancer have been recognized by the Urology community, as well as the WHO/AJCC classifications. These efforts have significantly “moved the needle” in the quest for more patient-centered diagnosis. Dr. Epstein obtained a combined BA-MD degree from Boston University’s 6-Year Medical Program (1975–1981). He undertook pathology training, first in anatomic pathology at The Johns Hopkins Hospital, followed by fellowship in oncologic surgical pathology at Memorial Sloan Kettering Cancer Center. At MSKCC, Dr. Epstein published works on prostatic “endometrioid” (i.e. ductal) and mucinous carcinomas, an early foray into clinicopathologic descriptions of variant entities. He was co-fellow with two budding pathologists who would become pillars of the MSKCC pathology community, Drs. Marc Rosenblum and Victor Reuter. Following fellowship, he returned to The Johns Hopkins Hospital, as chief fellow and subsequently as a staff member and has remained ever since. Dr. Epstein quickly rose through the academic ranks at Johns Hopkins to become Professor of Pathology, Urology, and Oncology. He is the recipient of the Reinhard Chair of Urological Pathology and long-time Director of Surgical Pathology and the GU Pathology service. Dr. Epstein joined the efforts to better characterize and understand the clinical implications of prostate cancer at a critical moment in prostate cancer history. His arrival “on the scene” of prostate cancer diagnosis converged with the advent of the PSA-era and his personal efforts, together with fruitful collaborations with Drs. Pat Walsh and Alan Partin, among other uro-oncology colleagues, led to major advances in prostate cancer diagnosis and patient care. Utilizing the expanding cohort of radical prostatectomy specimens at Johns Hopkins, Dr. Epstein began to explore the impact of prognostic factors, such as prostate cancer grade, stage, margin status and quantification on clinical outcomes, work that continues well into the current decade. His best known and most cited work however, is the landmark 1994 JAMA study, “Pathological and Clinical Findings to Predict Tumor Extent of Nonpalpable (stage T1c) Prostate Cancer,’’ which was the first to establish formal criteria for active surveillance. The “Epstein criteria” for active surveillance eligibility on prostatic needle biopsy and insignificant disease at radical prostatectomy, as well as his input in crafting the “Partin tables” for prediction of radical prostatectomy outcomes, are considered benchmarks against which contemporary predictive models are measured. In the late 1990’s and early 2000’s, Dr. Epstein’s efforts in defining the spectrum of prostate cancer variants and mimics continued unabated, including important clinicopathologic series on prostatic adenosis and foamy / atrophic / pseudohyperplastic cancers. Historically however, it might be recognized that his 2000 editorial, entitled “Gleason score 2-4 adenocarcinoma of the prostate on needle biopsy: a diagnosis that should not be made”, triggered a re-evaluation of Gleason grading, its reproducibility among experienced GU and community pathologists and its evolution in practice. This culminated in the 2005 International Society of Urological Pathology Consensus Conference on Gleason grading, at which the international GU Pathology community, reflecting large-scale empiric experience in clinical practice, codified changes to Gleason grading. This included near-total removal of cribriform carcinoma from pattern 3, a significant change which has been borne out by molecular genetic studies since that time. Having presided over the conference sponsored by the International Society of Urological Pathology, Dr. Epstein and colleagues introduced a modified prostate cancer grading diagram which reflected its results, while simultaneously initiating studies to clarify areas in which no consensus had been reached. During the ensuing decade his contributions included significant studies of intraductal carcinoma on needle biopsy, which highlighted this emerging entity and its clinicopathologic import to the pathology community. Seeking a more patient-focused system, in 2013, Dr. Epstein combined two significant paths of his career, prostate cancer grading and active surveillance criteria, proposing a system of prognostic grade groups, which would have the effect of simplifying clinical management conversations in very low and low risk cancers such that patients could be treated as grade group 1, rather than Gleason score 6/10. This was quickly followed by multi-institutional validation and formed much of the substance of the 2014 International Society of Urological Pathology Conference on Prostate Cancer Grading, following which grade grouping has become a standard reporting element, adopted by WHO/AJCC classifications, as well as CAP and ICCR reporting protocols. In the past 35 years, Dr. Epstein has parlayed his vast experience at Johns Hopkins and in consultation (approximately 12,000 cases per year) to publish over 900 peer-reviewed manuscripts (over 600 in the realm of prostate cancer alone!). These, as well as numerous texts and textbook chapters, including his Prostate (w/George Netto) and Bladder (w/Victor Reuter & Mahul Amin) Biopsy Diagnostic Interpretation guides are standard texts on GU Pathology and resident/fellow bookshelves. Not as well known, is that Dr. Epstein routinely signs out General Surgical Pathology as part of the Johns Hopkins team. Concurrently, he has run a GU Pathology fellowship for nearly 25 years, training nearly 65 fellows over that period, many of whom are established or emerging leaders in the next generation of GU Pathology. He is a gifted and efficient teacher, pioneered early online image databases for improving prostate and bladder grading reproducibility, and not surprisingly, has received numerous awards, including from the Arthur Purdy Stout Surgical Pathology Society, the International Society of Urologic Pathology (which he also served as President and founder of its website) and multiple Johns Hopkins Hospital Departmental Teaching Awards. As importantly in the realm of advancing clinical medicine, Dr. Epstein is also is a sought-after reference and speaker amongst the clinical urology and urologic oncology communities. Today, as we celebrate the memory of Dr. Fred Waldorf Stewart, a pathologist, who in his time, made significant contributions to the care of cancer patients, we are proud to bestow this year’s Award on a former MSKCC Oncologic Surgical Pathology fellow and leader in his field, Dr. Jonathan I. Epstein, who is supremely deserving of recognition for his immense contributions to the surgical pathology of the GU tract and specifically, prostate cancer and its clinical ramifications. We congratulate Dr. Epstein on this well-deserved award.
2017 Recipient
Andreas Helmut Robert von Deimling, MD
Dr. Andreas von Deimling is the 2017 recipient of the Fred Waldorf Stewart Award, bestowed annually by the Department of Pathology at Memorial Sloan Kettering Cancer Center on an individual who has made outstanding contributions to the characterization of human neoplastic disease. Honored for his efforts in the field of tumors involving the central nervous system (CNS) and it coverings, Dr. von Deimling currently serves as Chairman of the Department of Neuropathology at the University of Heidelberg, Germany (his home country) and as Founding Director of the Clinical Cooperation Unit (CCU) in Neuropathology under the auspices of the German Cancer Center (Deutsches Krebsforschungszentrum). Dr. von Deimling took his MD at the University of Freiburg, interrupting his studies there for two forays into laboratory- based research that bore early witness to his academic leaning. The first of these, in 1983, was to the famed Medical Research Centre Harwell (United Kingdom), an enterprise dedicated to the study of murine genetics and headed at the time by Mary Lyon (she of the Lyon hypothesis of X chromosome inactivation). Working under the direction of Dr. Jo Peters, Dr von Deimling there mapped the mouse biliverdin reductase gene. One year later, he travelled to the United States to work at the National Institutes of Health in the laboratory of Dr. Michael Potter, who had developed mouse models of plasmacytoma and who would win the Albert Lasker Basic Medical Research Award for fundamental investigations into immunoglobulin genetics that paved the road to hybridoma technology. It was there that Dr. von Deimling, under the tutelage of Dr. Konrad Huppi, had his first direct contact with molecular genetic methods. In 1988, Dr. von Deimling commenced training as a Resident in the Department of Neuropathology at the University of Zurich, Switzerland under the distinguished Paul Kleihues. From those days date his earliest first-author efforts in the human brain tumor area, studies investigating the histogenesis and differentiating potential of central neurocytomas. Not knowing the precise uses to which such materials would be placed but realizing that assays of potential research interest such as Southern and Western blotting required non-fixed tissues, trainee von Deimling took it upon himself to begin systematically freezing CNS tumor samples coming from the operating rooms. This must figure among the earliest efforts in brain tumor banking and would pay high dividends in the years to come, but it was an exasperated Professor Kleihues who wondered at the diminishing size of formalin-fixed, paraffinized tumor sections crossing his microscope for diagnosis. Dr. von Deimling’s intellectual restlessness had him interrupting his residency and, in 1990, again making for the United States, this time to the laboratory of Dr. Bernd Seizinger in the Department of Neurosurgery and Molecular Neuro-Oncology at the Massachusetts General Hospital / Harvard Medical School. The experience determined the path of his subsequent career as an academic neuropathologist principally focused on the molecular genetics of primary brain tumors. In Boston, Andreas met and partnered with Dr. David Louis, embarking on large-scale loss of heterozygosity (LOH) studies that employed the brain tumor samples collected in Zurich. The pair and their co-workers, among many original observations, would implicate chromosome 19q in the pathogenesis of diffuse gliomas and demonstrate the consistent association of allelic losses involving this and chromosome 1p with tumors exhibiting the histology of oligodendroglioma or oligoastrocytoma. Most readers will be aware that chromosome 1p/19q co-deletion is now a defining feature of “canonical” oligodendrogliomas as codified in the 2016 World Health Organization (WHO) taxonomy of CNS neoplasms. Noteworthy as well from this period is a study so novel at the time that von Deimling and colleagues had great difficulty getting it published. It is hard to fathom the resistance they met now, as the work demonstrated that glioblastomas, recognized as heterogeneous in their clinical biology and histology, could be subdivided into molecular genetic subsets. Following his sojourn in Boston, Andreas returned to Germany, completing his training as a Resident in the Department of Neuropathology at Bonn where he was mentored by renowned Professor Otmar D. Wiestler and awarded the Hermann and Lilly Schilling Professorship. After several highly productive years as a Consultant in that department, Dr. von Deimling went on to assume Directorship of the Department of Neuropathology, Charite, Berlin (1998-2006) before being recruited to his current Chair position at Heidelberg. The effort to create the interdisciplinary CCU Neuropathology was initiated when Andreas accepted the Heidelberg offer. He assumed personal responsibility for the recruitment of its members, who under his direction now constitute a team unrivalled in the defining of adult and pediatric brain tumors as molecular genetic entities and, of particular relevance to the award memorializing Fred Stewart, in the development of diagnostic tools for use by pathologists the world over. Tradition demands of those composing academic encomia that the honoree’s tally of peer-reviewed publications be provided, as if that number alone could stand guarantee of the subject’s impress. Very well. We hover near 500 and, yes, these have regularly appeared in the most demanding and influential of periodicals. Dr. von Deimling’s investiga - tions have ranged over the spectrum of neuroepithelial, meningothelial and mesenchymal neoplasms affecting children and adults, delineating genetic and epigenetic profiles that are now recognized as characteristic of diffuse gliomas, ependymomas, medulloblastomas and other embryonal tumors, choroid plexus tumors, meningiomas and neoplasms of peripheral nerve sheath origin. A close parsing of these contributions is beyond the confines of this sketch and so the writer has decided to invoke the spirit of Stewart himself and limn those works accomplished by von Deimling and his CCU Neuropathology that have come to bear specifically on the practice of surgical neuropathology and that suggest the future course of this subspecialty. Following the discovery of isocitrate dehydrogenase (IDH) mutations in a subset of glioblastomas, Dr. von Deimling and team demonstrated a high incidence of IDH1 codon 132 mutations in diffuse astrocytomas and oligodendrogliomas (WHO grade II and III) as well as “secondary” glioblastomas arising in young individuals. These proved foreign to neuroepithelial neoplasms of other types and to reactive processes. In 2009, his group announced the development of a sensitive and specific antibody to IDH 1 R132H, the isoform accounting for approximately 90% of all mutant IDH species encountered in diffuse gliomas. The use of this commercially available reagent rapidly assumed standard-of-practice status in pathology laboratories the world over, as the immunohistochemical demonstration of IDH1 R132H labeling came to be accepted by both basic and clinical neuroscientists, neurooncologists included, as proof positive of this specific mutational event. The application of this single reagent to the analysis of neurosurgical material potentially allows even the unpracticed observer to identify a glial proliferation as neoplastic rather than hyperplastic, to assign the tumor thus identified to the diffuse glioma series, and to convey information of substantial prognostic and predictive import (IDHmutant gliomas are considerably less aggressive than their wild-type counterparts and IDH inhibitors are in clinical trial for affected patients; in fact, von Deimling and crew have recently developed and characterized a novel pan-mutant IDH1 inhibitor that they have shown to be active against human IDH-mutant astrocytomas). The Heidelberg team subsequently threw down strong challenges to the legitimacy of traditional histologic grading when divorced from an assessment of IDH status, showing that most IDH wild-type astrocytomas qualifying for WHO grade II designation actually have molecular genetic signatures associated with glioblastomas, generally behaving as such, and, in retrospective analyses, demonstrating that comparable outcomes attach to IDH-mutant astrocytomas classified as WHO grade II or III. This neuropathologist hasn’t a colleague who does not employ the anti-mutant IDH1 antibody in a simple diagnostic algorithm (or some variant thereof ) proposed by Dr. von Deimling and company for the subclassification of diffuse gliomas into molecularly distinct and clinically relevant entities. The successes detailed above were repeated in 2011 when the von Deimling group announced the development of an antibody specifically identifying BRAF v600E, a mutant BRAF species encountered in a variety of extraneural tumors that prominently includes cutaneous melanomas, papillary carcinomas of the thyroid gland, Langerhans cell histiocytosis, Erdheim-Chester disease and, at lower frequency, borderline ovarian tumors and colorectal adenocarcinomas. Andreas and co-workers would go on to demonstrate BRAF v600E mutation in most pleomorphic xanthoastrocytomas and in a significant subset of gangliogliomas, the roster of potentially BRAF v600E-mutant brain tumors now including “epithelioid” glioblastomas, pilocytic astrocytomas, a variety of low-grade glial and glioneuronal neoplasms seen mainly in the young, and papillary craniopharyngiomas. This reagent has become a staple of practice across pathologic subspecialties for its obvious value in matters of tumor subclassification and in identifying candidates for BRAF inhibitor treatment. Andreas and colleagues have also demonstrated that meningeal hemangiopericytomas and solitary fibrous tumors constitute an entity unified by NAB2- STAT6 gene fusions, as displayed by their extraneural counterparts, and have proven the value of nuclear STAT6 overexpression as an immunohistochemical phenomenon reliably distancing such lesions from meningiomas and other neuraxial mimics. Recent efforts by Dr. von Deimling and the Heidelberg team address epigenomic brain tumor profiling. Utilizing an expansive and carefully annotated collection of neoplasms, the group demonstrated that entities having established histologic features, genetic abnormalities and patterns of gene expression also have identifying signatures on CpG methylation array. Andreas and co-workers then developed a CpG methylation array-based algorithm for purposes of tumor classification that they offered to apply gratis to tumor samples sent them by pathologists practicing anywhere in the world. This powerful technology has proved capable not only of accurately pigeon-holing many neoplasms of poorly differentiated or otherwise ambiguous morphology, but suffices to identify clinically relevant subtypes within tumor categories (e.g., Wnt or SHH-driven medulloblastomas, RELA- fused ependymomas and C19MC- altered embryonal tumors with multilayered rosettes). Methylation array profiling also played a major role in the recent identification of several novel entities hidden under the obscuring rubric of “primitive neuroectodermal tumor”. MSKCC is hardly first in recognizing Dr. von Deimling’s outsized role in brain tumor characterization and in shaping the careers of younger investigators in the field. An elected Fellow of the European Academy of Cancer Sciences, he has delivered the A. Julio Martinez Lecture (created by the Department of Pathology at the University of Pittsburg School of Medicine to memorialize the great Cuban-born neuropathologist), has won the Abhijit Guha Oration Award (bestowed by the Indian Society of Neuro-oncology in memory of the skilled neurosurgeon and investigator who figured prominently in the establishment of a National Neurosciences Centre in his native Kolkata), and is the recipient of the Dorothy S. Russell Medal (given by the British Neuropathological Society in celebration of the towering figure who coauthored Russell and Rubinstein’s classic Pathology of Tumors of the Nervous System and who was the first woman to be appointed to a pathology chair in Western Europe). In 2016, Andreas collected the prestigious German Cancer Prize (Deutscher Krebspreis) in the translational research division. He was also recruited by the WHO as a senior advisor to the formulation of the revised 4th edition of the “blue book”, WHO Classification of Tumours of the Central Nervous System (2016), a work that broke with a century of tradition by departing from the exclusively morphologic and building molecular genetic characteristics into the very definition of select entities. Dr. von Deimling must now make room in his trophy case for the Fred Waldorf Stewart Medal. That “the old man” approves is a surety. While rightly revered as a preternaturally gifted morphologist, Dr. Stewart, as dean of tumor pathologists, as James Ewing’s successor to the Chair of Pathology at Memorial Hospital and Founding Editor of the journal Cancer, advocated throughout his career for the application of novel technical methods to the study of neoplastic disease. In this, he was propelled by that curiosity which has ever informed the creative and which was enunciated by one of Dr. von Deimling’s great countrymen thus: “Thinking is more interesting than knowing, but less interesting than looking.” Goethe To which we can only add- Keep looking, Andreas. Keep looking. Marc K. Rosenblum, MD
2016 Recipient
Ralph Hruban
Ralph Hruban is a world-renowned pancreatic cancer pathology expert who has devoted his academic career to the study of pancreatic neoplasms. He has made significant contributions to the understanding of all types of pancreas tumors: ductal, acinar, and neuroendocrine. Importantly, his work on pancreatic intraepithelial neoplasias (PanINs) and intraductal papillary mucinous neoplasms (IPMNs), the precursor lesions that give rise to invasive pancreatic cancer, has had a particularly significant impact both in the field of pancreas research and with regard to how patients are prognosticated and managed.
Dr. Hruban obtained his undergraduate degree from the University of Chicago and his medical degree from the Johns Hopkins University School of Medicine. His pathology training consisted of residency in anatomic pathology at Johns Hopkins and fellowship in oncologic surgical pathology at Memorial Sloan Kettering Cancer Center. In 1990, upon completion of his fellowship, Dr. Hruban returned to Johns Hopkins to join the faculty and has remained there ever since. Quickly rising through the academic ranks to become professor of both pathology and oncology, Dr. Hruban has served multiple important roles over the years at Johns Hopkins, and is currently Director of the Sol Goldman Pancreas Cancer Research Center, Director of the Division of Gastrointestinal and Liver Pathology, and Director of the Department of Pathology.
Dr. Hruban joined the quest to conquer pancreatic cancer early on. In the early 1990s, the world of biomedical research was in one of its more visible transformations from older-style analyses to newer and more complex technologies, and the focus on the origins of cancer was converging at the molecular level largely as a consequence of studies done with the newer technologies. It was then that Dr. Hruban and his colleagues took to techniques such as mutant-enriched polymerase chain reaction analysis in combination with allele-specific oligonucleotide hybridization, and revealed that KRAS mutations (now known to represent one of the few big “mountains” in pancreatic cancer’s genomic landscape) were important events in the disease. Dr. Hruban envisioned presciently then that specific molecular alterations of this type would not only allow a better understanding of the genetic drivers for pancreatic cancer development, but also have the potential to serve as markers for the detection of this deadly disease at an early stage when intervention might still save lives. In the same spirit of applying innovative approaches to the study of cancer, Dr. Hruban also co-founded the National Familial Pancreas Tumor Registry at Johns Hopkins, a patient registry that would now serves as an invaluable resource for the study of pancreas tumors.
The two decades following these initial efforts saw Dr. Hruban diving ever deeper into the field of pancreas neoplasia, while keeping focus on understanding the noninvasive precursor lesions from which invasive cancers develop (PanINs and IPMNs), the familial aggregation of some pancreatic cancers, and the pathologic ramifications of genetic alterations in the pancreas. During this time, at Hopkins and with multi-institutional collaborative groups, Dr. Hruban produced meritorious scientific work that served both to advance pancreatic cancer research as well as to facilitate diagnosis, detection, prevention, prognosis and treatment. In testament to such achievements, Dr. Hruban has over 700 scientific papers, and is cited by the Essential Science Indicators as the most cited pancreatic cancer scientist in the world. It is only natural that numerous awards have been bestowed on him in recognition of his achievements, including the Arthur Purdy Stout Prize and the Ramzi Cotran Award from USCAP, the PanCAN Medical Visionary Award, the Ruth C. Brufsky Award of Excellence in Clinical Research for Pancreatic Cancer, and election to the German National Academy of Sciences Leopoldina. Most recently, riding on the wave of next generation sequencing, Dr. Hruban, along with a group of distinguished pancreas scientists including MSK’s Christine Iacobuzio-Donahue made the discovery of a new cancer pathway and new familial pancreatic cancer genes, defined the time course for the development of pancreatic neoplasia, and showed that each of the four cystic tumors of the pancreas has a unique mutational profile. Once again, these efforts have significantly improved the understanding of the fundamental genetic changes that characterize pancreatic neoplasms, and importantly, bear immediate clinical implications. It is only fitting that Dr. Hruban and his colleagues were recognized for their efforts as recipients of the prestigious Team Science Award from the American Association for Cancer Research.
Dr. Hruban is also a superb surgical pathologist and an ardent educator. He has dedicated time and effort to the teaching of gastrointestinal and pancreas pathology to trainees and practicing pathologists as well as patients worldwide. He has disseminated knowledge through lectures, courses, books, and digital media. Dr. Hruban has written more than 150 book chapters and reviews, and authored or coauthored six books, including the AFIP Fascicle on Tumors of the Pancreas and the World Health Organization “blue book” on tumors of the digestive tract. With a deep appreciation of visual arts, Dr. Hruban has utilized creative images for the teaching of pathology and developed iPhone and iPad apps to teach pancreas pathology to medical professionals and to serve as an educational guide for patients, family members and friends facing a diagnosis of pancreatic cancer.
Dr. Hruban has also made his mark in other fields, as he has produced an award-winning documentary on William Stewart Halsted and an audio series called “Osler Minutes” on the philosophy of William Osler.
Previous Recipients
- Frank W. Foote, MD (1978)
- A.G. Everson Pearse, MD (1979)
- Robert E. Scully, MD (1980)
- Raffaele Lattes, MD (1981)
- William M. Christopherson, MD (1982)
- Hans Popper, MD (1983)
- Leopold G. Koss, MD (1984)
- Franz M. Enzinger, MD (1985)
- Arthur C. Upton, MD (1986)
- Lauren V. Ackerman, MD (1987)
- David C. Dahlin, MD (1988)
- Peter C. Nowell, MD (1989)
- Renato Baserga, MD (1990)
- Javier Arias Stella, MD (1991)
- Karl Lennert, MD (1992)
- Myron R. Melamed, MD (1993)
- J. Bruce Beckwith, MD (1994)
- John F.R. Kerr, MD (1995)
- Lance A. Liotta, MD (1996)
- Sharon Whelan Weiss, MD (1997)
- John J. Kepes, MD (1998)
- Ronald A. Delellis, MD (1999)
- John Aidan Carney, MD (2000)
- Stephen S. Sternberg, MD (2001)
- Elaine S. Jaffe, MD (2002)
- James M. Woodruff, MD (2003)
- William Jackson Frable, MD (2004)
- Christopher D.M. Fletcher, MD (2005)
- Juan Rosai, MD (2006)
- Peter C. Burger, MD (2007)
- Paul Peter Rosen, MD (2008)
- Robert J. Kurman, MD (2009)
- Julia A. Bridge, MD (2010)
- Stanley R. Hamilton, MD (2011)
- E. Leon Barnes, MD (2012)
- Richard Kempson, MD (2013)
- Thomas M. Ulbright, MD (2014)
- Robert H. Young, MD (2015)