Rebecca Lerner receives a chemotherapy infusion at MSK. She was diagnosed with colorectal cancer just before she turned 33.
A disturbing question lies at the heart of a common and deadly cancer. Why is colorectal cancer striking more people as young as their 20s and 30s — and even teenagers?
Most of these young people have no family history of the disease. They also have few of the risk factors associated with colorectal cancer, which typically develops in people 60 and older.
In fact, many of the clues that medical investigators rely on have led to dead ends.
First Center in the World
To find answers, Memorial Sloan Kettering Cancer Center established the first center in the world devoted to the specific needs of people under 50 with these cancers.
Since March 2018, specialists at the MSK Center for Young Onset Colorectal and Gastrointestinal Cancer have cared for more than a thousand young people — body and soul.
The Center is also a focal point for a massive research effort that flows back and forth from MSK patient beds and clinical trials to laboratories and sophisticated artificial intelligence tools at the Sloan Kettering Institute (SKI).
The goal of this collaboration is to translate MSK’s unparalleled expertise into advances that will save lives.
A Terrible Trend
The statistics are startling: For the past few decades, the number of people below age 50 who are diagnosed with colorectal cancer has been steadily rising. In fact, cases of the disease among younger adults are expected to nearly double by 2030.
Even worse, the death rate from colorectal cancer for younger people is ticking upwards, after previously declining for years.
A More Aggressive Cancer?

Andrea Cercek is Co-Director of the Center for Young Onset Colorectal and Gastrointestinal Cancer.
Medical oncologist Andrea Cercek is Co-Director of MSK’s Center along with gastroenterologist Robin Mendelsohn. Dr. Cercek says, “One of the most urgent questions we needed to answer is how we should treat these younger patients.”
She explains: “Does the rise in colorectal cancer in younger people signal that the disease is more aggressive in these patients and should be treated more aggressively too? Is this a new kind of colorectal cancer?”
Dr. Cercek adds that “many doctors decided that since younger patients are usually stronger than older patients, it made sense to treat them with stronger chemotherapy regimens.”
‘Happening Earlier’
However, important new translational research at MSK suggests a new way forward. In a paper published in August 2021, Dr. Cercek and her research group, including MSK’s computational biology team, performed the largest and most comprehensive comparison ever of colorectal patients below 50 — and as young as their teens — with patients over 50.
The comparison of 1,446 MSK patients looked at the genomic makeup of patient tumors, the different areas in the colon and rectum where the tumors developed, the treatments that were given, and the outcomes of each age group, including overall survival rates.
“We found there are really no differences, across the board, no matter how old or young a patient is,” says Dr. Cercek. “This is the same disease biology in younger patients — it’s just happening much earlier in their lives.”
Dr. Cercek adds: “Importantly for younger patients, we also found that their responses to chemotherapy are the same as older patients and so are their survival and outcomes.”
What that means, she says, is “we should not treat these patients differently just because they’re young, because it won’t improve their outcomes. They will just have more toxicity without any benefits.”
She concludes, “Since our research suggests this disease is the same across all age groups, the next question we’re trying to answer is, ‘Why is this happening to younger people?’ ”
The hunt for clues is taking place in clinics and labs across MSK, including a collaboration between Dr. Cercek and MSK medical oncologist Rona Yaeger, a physician-scientist. Together with other colleagues, one aspect they are investigating is the genetic evolution of colorectal cancer in young people.
Translating Cancer’s Cross Talk
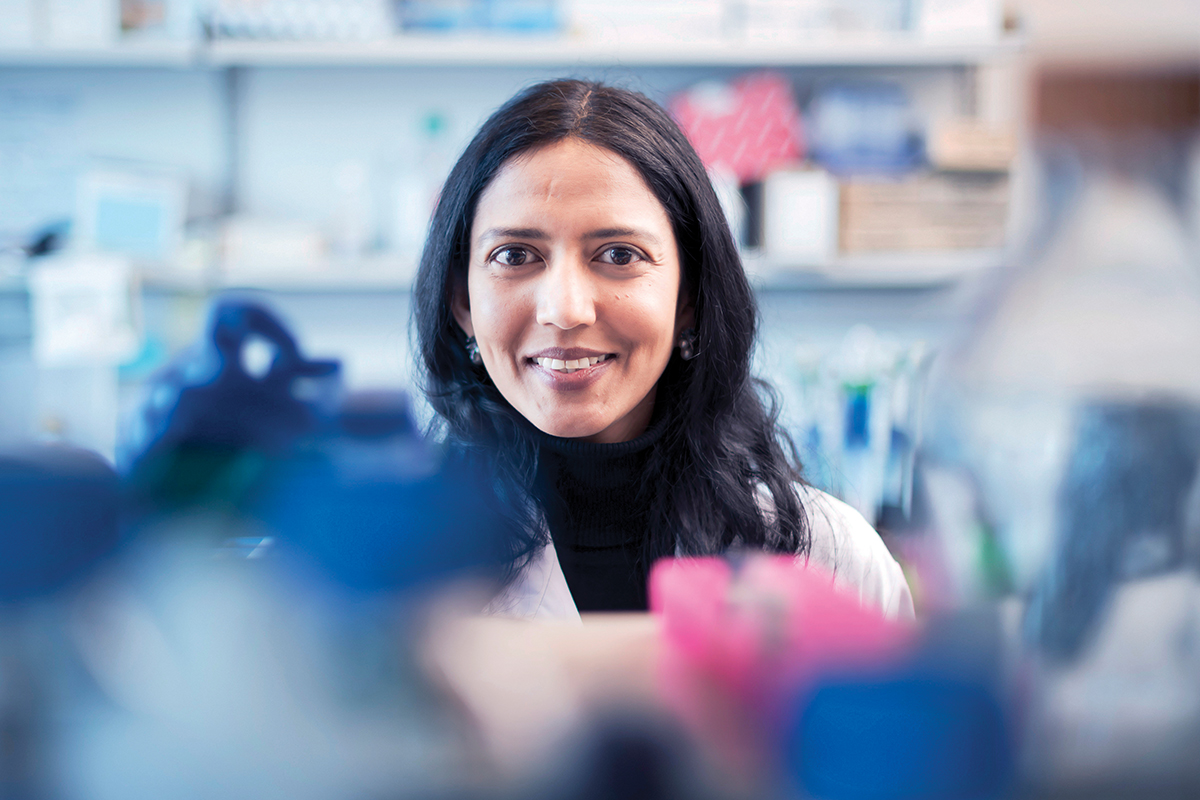
Physician-scientist Karuna Ganesh is a member of the Molecular Pharmacology Program at the Sloan Kettering Institute.
Another place searching for answers is the SKI laboratory of Josie Roberston Investigator Karuna Ganesh. She is a physician-scientist who cares for patients with gastrointestinal cancers and is a member of the Molecular Pharmacology Program at SKI.
She stresses that at SKI, researchers are investigating cancer from every angle. “We are looking not just at the tumor in isolation but at systemic factors, meaning things that are happening in the whole body that influence how the tumor can survive.”
She explains that systemic factors “include the immune system, hormones, and signals from nerves and how these interact with cancer cells, as well as the microbiome” — the enormous community of bacteria and other organisms living in our bodies that play a significant role in our health. “We also look at how all of these factors are influenced by diet and exercise, age, and medications a person is taking.”
The goal, she says, is to understand the “cross talk that happens among these systemic factors and cancer cells, so we can tease apart the mechanisms by which cancer arises and grows.”
Rise of the Organoids
A powerful method to eavesdrop on this cross talk is called an organoid. Dr. Ganesh describes an organoid as a “mini gut, where cells from a patient’s tumor are grown in a dish in three dimensions, so you see all of the different cell types just like in an intact tumor.”
The organoid “can also evolve and change to respond to different stresses and environmental signals, just like a primary tumor or metastatic cancer cells that have spread.”
This ability for cancer cells to adapt to changing environmental cues is called plasticity, and it’s an important reason that many cancer treatments lose their potency over time in some patients, as tumor cells evolve to outwit the therapy.
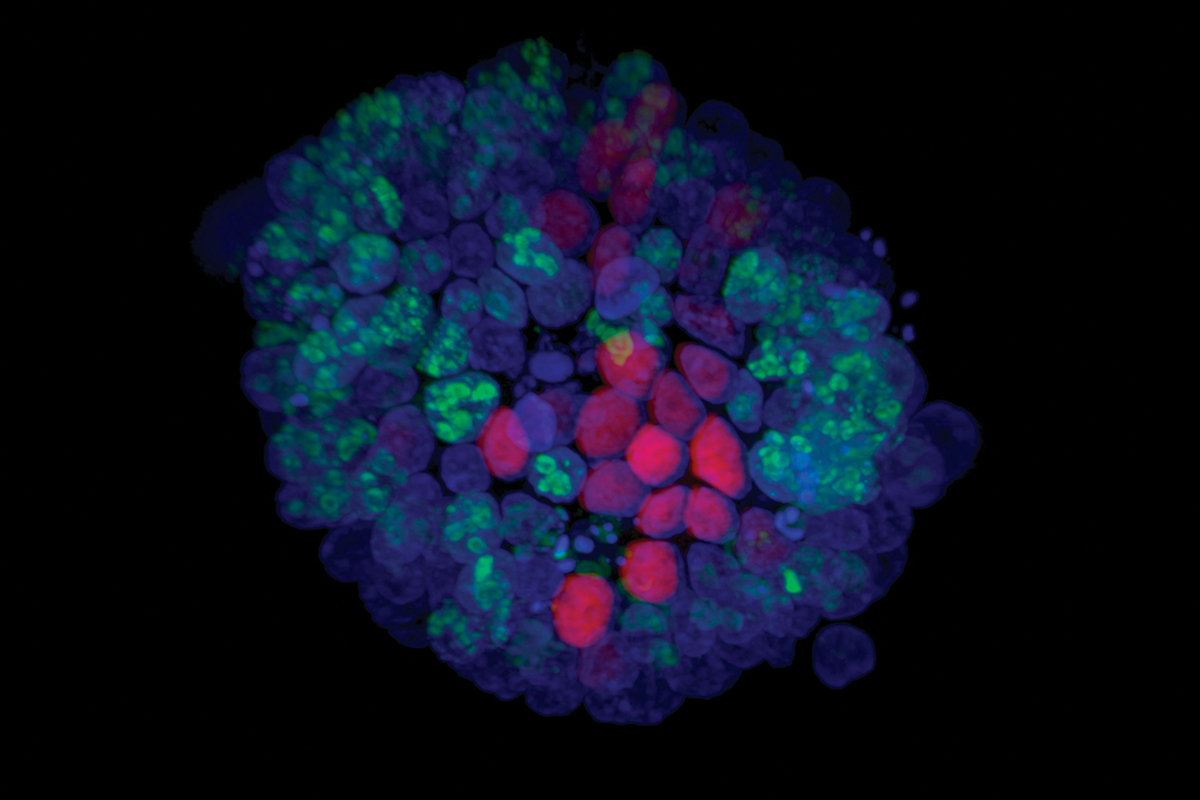
This colorectal cancer organoid shows dividing tumor cells (in green) and nondividing tumor cells (in pink).
By introducing a patient’s own microbiome and immune cells into the organoid, Dr. Ganesh and her team can see how all the cells interact with the tumor.
Dr. Ganesh says the insights that have been gained prove the value of translational research at MSK. “Unlike traditional cancer models, studying patient samples and organoids enables us to capture the diversity and plasticity of tumor and environment interactions that we see in our patients. Ultimately, our goal is to use these insights to develop more effective drugs to treat cancer. This is why the translational research effort that spans the clinic and the lab is so important.
Dr. Ganesh is also quick to point out that “trying to understand the interplay of so many different factors probably would not be possible, to be honest, without the collaboration of our SKI colleagues in computational biology, like Dana Pe’er and Christina Leslie.”
360-Degree View of Cancer
This 360-degree view of cancer is also the bedrock of the Center for Young Onset Colorectal and Gastrointestinal Cancer, which aims to help people with the specific issues they face at a particularly vulnerable stage of life.
Rebecca Lerner found out she had colorectal cancer in early 2021, just weeks before her 33rd birthday. She had insisted on a colonoscopy after years of persistent stomach issues.
Neither she nor her healthcare providers thought someone so young and healthy could have colon cancer — a common obstacle to early diagnosis for young people who develop the disease.
“There’s nothing like being told you have cancer,” she recalls. “You don’t know how to function.” When she learned she had stage 3 colon cancer, she says, “I went to the darkest places my mind has ever been.”

Ian and Rebecca Lerner walk through New York’s Soho neighborhood on their wedding day. Photo by @stephmannphotography.
Swinging Into Action
After surgery at a major hospital near her home in New Jersey, Rebecca came to MSK for chemotherapy. Her age and diagnosis meant the Center was alerted as soon as she made an appointment.
Behind the scenes, specialists at the Center who had treated many young people like Rebecca swung into action.
“I met with Dr. Cercek for the first time on March 3 of 2021. I told her my fiancé and I had set our wedding date for the next week — was that OK? She said, ‘It’s perfectly OK.’ ”
She continues, “Then Dr. Cercek and the Center immediately began to help me with fertility preservation so I could freeze my eggs before starting chemo. My husband, Ian, and I both hope for a family of our own, so we froze embryos as one option for having children. I was so relieved all of this was just automatically part of the plan for a younger person like me. I don’t think it would be like this at other hospitals.”
Best Care
After Rebecca’s first appointment, the Center’s dedicated social worker — Hadley Maya — reached out to Rebecca, as she does with all the Center’s patients.

MSK social worker Hadley Maya
“She saved me,” Rebecca says. “I wanted her to be my best friend. I think she is my best friend,” Rebecca admits with a laugh — “she just doesn’t know it.”
Rebecca credits Hadley with helping her through a challenge that may be unique to younger cancer patients. “I got married in the middle of all this, and while I’m fortunate to be very close with my parents, it created some difficult dynamics. I needed to do this with my husband — he had to be my caregiver — without hurting my parents’ feelings. Hadley helped me navigate the relationship with my parents, so that everyone felt heard.”
Today, Rebecca has no evidence of disease. And she remains in close touch with her care team at MSK, explaining, “They do all of the things that you need, and the things you don’t know you need. I feel like I got the best care possible because of it.”