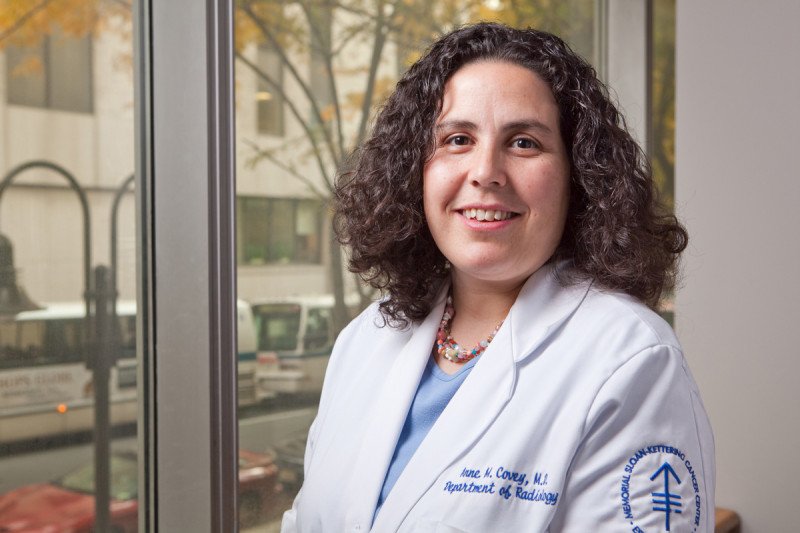
MSK interventional radiologists like Anne Covey use minimally invasive therapies to treat small liver tumors effectively with fewer complications than surgery.
Treating liver cancer and liver metastases — cancer that has spread to the liver from elsewhere in the body — is challenging. Most patients are not candidates for surgery because of either the number or location of tumors.
In some cases, however, tightly focused, minimally invasive therapies can treat liver tumors effectively. With this approach, called interventional radiology (IR), physicians use imaging guidance paired with tools such as needles and catheters to pinpoint the exact area for treatment.
At Memorial Sloan Kettering, interventional radiologists do nearly 14,000 procedures each year, including over 500 to treat liver cancers. Imaging techniques such as CT scans, ultrasound, PET, and MRI enable interventional radiologists to target tumors and destroy them.
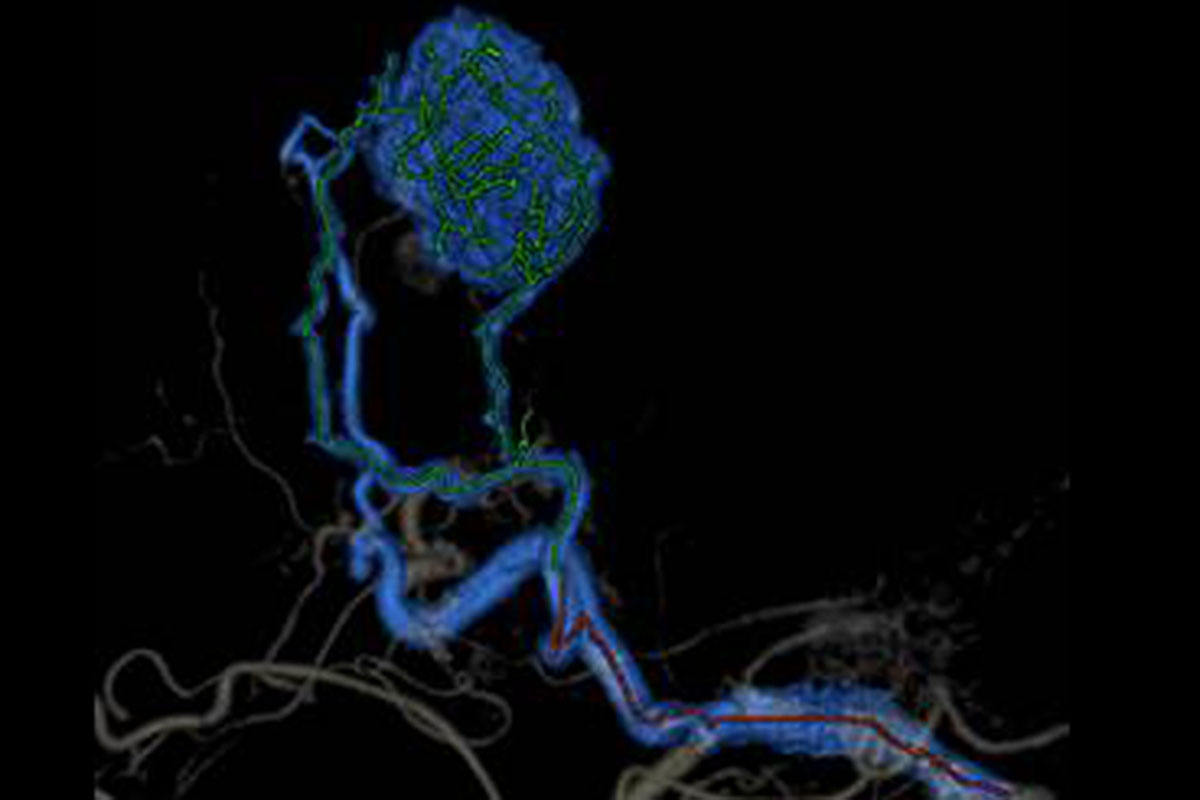
Imaging reveals blood vessels (blue and green) that supply a liver tumor (at top). Interventional radiologists can use a procedure called an embolization to choke off the blood supply and kill the tumor. Image courtesy of Anne Covey
“For certain types of cancer, we can use interventional radiology techniques, which compared to surgery, are a lot easier to tolerate,” says MSK interventional radiologist Anne Covey. “Patients tend to have fewer complications and a faster recovery. Often our patients go home the same day or the day after a procedure.”
Dr. Covey and her IR colleagues treat both primary and metastatic liver cancers. The most common primary liver cancers are hepatocellular carcinoma, which arises in the liver, and cholangiocarcinoma, which starts in the bile duct. Metastatic liver cancers usually have spread to the liver from the colon or breast. Another metastatic liver cancer sometimes treated with IR is a rare disease called neuroendocrine tumors, which begin in specialized cells called neuroendocrine cells and can arise from anywhere in the body, most typically the pancreas, intestine, or lung.
“People with liver cancer often have cirrhosis [scarring] — it’s often what caused the tumor to develop — so you’re treating two diseases at the same time,” Dr. Covey says. “This can make surgery unsafe because of the risk of liver failure in patients with compromised liver function. And systemic therapy, where you take a pill or have chemotherapy intravenously, affects the entire body. Using IR lets us limit the treatment to where the tumor is.”
Embolization: Blocking Fuel Lines
The most commonly used IR approach for liver tumors at MSK is embolization. This involves injecting microscopic beads — with diameters roughly the width of a human hair — into the blood vessels that feed the liver tumors. Sometimes the goal is simply to choke off the blood supply to the tumor and kill it, a technique called bland embolization. Among cancer types, primary liver tumors and neuroendocrine tumors are especially dependent on an ample blood supply, so bland embolization can be particularly effective.
The beads can also be filled with chemotherapy to shrink or kill the tumor, but Dr. Covey says MSK has not used the approach much for liver tumors. “For liver cancer, we have shown that adding chemotherapy doesn’t improve outcomes compared with bland embolization,” she explains. “The added chemotherapy can also cause side effects and scarring of the arteries, making it harder to do future treatments of the tumor if needed.”
The IR specialists do sometimes add radiation to the beads, known as radioembolization or Y90 treatment, for patients with liver metastases from the colon and breast and neuroendocrine tumors. Some patients who have had previous surgery involving the bile ducts are at high risk for infectious complications.
For example, patients with a pancreatic neuroendocrine tumor may have had a Whipple procedure, which involves removing the tumor and then reattaching the bile duct to the bowel. Radioembolization appears to reduce the risk of infections in these patients compared with bland embolization, Dr. Covey says.
Repeat embolization procedures are common. “With embolization alone, we’re rarely achieving a cure but hope to kill most tumor cells in the area,” Dr. Covey says. “We monitor these people very closely, with CT or MRI scans every three to six months, typically for the rest of their lives. If the cancer grows back, we can treat it again.”
Direct Destruction
The other main IR approach for liver tumors is ablation. This involves placing a specialized needle, or probe, into the tumor and destroying it by freezing it (cryoablation) or using radio waves (radiofrequency ablation) or microwaves (microwave ablation) to superheat the tumor. IR specialists also can destroy tumors by injecting cancer-killing chemicals, such as pure alcohol (ethanol) or acid, directly into them.
For some liver tumors previously not able to be treated with ablation because of location near bile ducts or blood vessels, IR specialists may use electrical currents (called irreversible electroporation) to punch holes in cancer cell membranes to kill a tumor. The instrument used for this is called a NanoKnife®.
“Ablation is exciting because it is potentially curative,” Dr. Covey says. “We can completely obliterate the tumor with results that are comparable to surgery. At the same time, it’s limited in application. It’s really appropriate only in people whose liver tumors are very small in size and number.”
Team Approach
Dr. Covey says IR is just one component of MSK’s collaborative process, which ensures patients receive the best treatment for their specific case. “I can’t think of any person with liver cancer who is managed by only one specialist in this institution,” she says. “There’s always an entire disease management team evaluating their case and guiding them through treatment. This could include an oncologist, a hepatologist, a gastroenterologist, a surgeon, a radiation oncologist, and an interventional radiologist. It makes an enormous difference in their treatment and outcome.”
Another advantage is the state-of-the-art facilities that make these collaborations possible. Most procedures are done in MSK’s Center for Image Guided Intervention (CIGI) in Memorial Hospital. CIGI has six procedure rooms with highly advanced imaging equipment. An increasing number of patients receiving IR for liver cancer are also seen at the David H. Koch Center for Cancer Care at Memorial Sloan Kettering, which opened in early 2020.
“Both of these beautiful facilities make the experience more comfortable for patients,” Dr. Covey says. “This is especially true when it comes to privacy following the procedure — people have their own bay or even their own room to recover. Our goal is to use this technology to get them back to their daily lives as fast as possible.”